在线提供 29 June 2022
Abstract
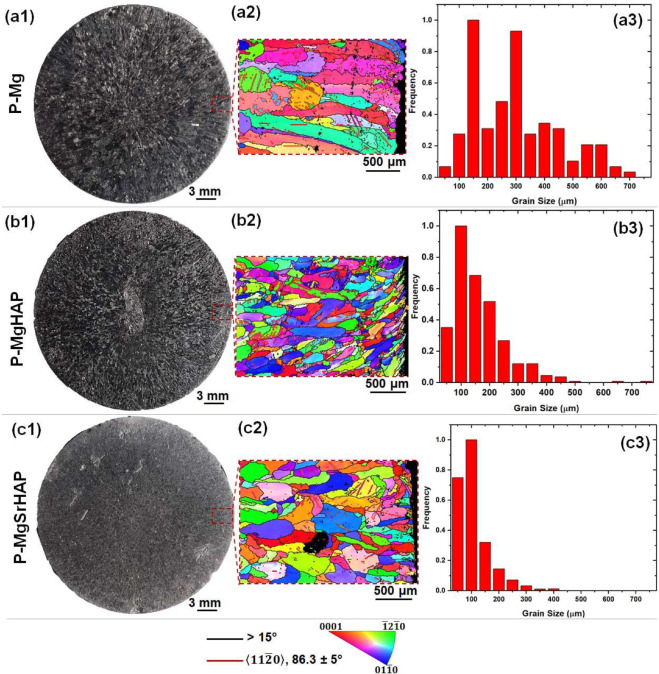
Magnesium-based
biomaterials have been in extensive research for orthopedic
applications for decades due to their optimal mechanical features and
osteopromotive nature; nevertheless, rapid degradation restricts their
clinical applicability. In this study, pristine magnesium was purified
(P-Mg) using a melt self-purification approach and reinforced using
indigenously synthesized nanohydroxyapatite (HAP, 0.6 wt.%) and
strontium substituted nanohydroxyapatite (SrHAP, 0.6 wt.%) using a
low-cost stir assisted squeeze casting method to control their
degradation rate. Using electron back-scattered diffraction (EBSD) and
X-ray diffraction (XRD) examinations, all casted materials were
carefully evaluated for microstructure and phase analysis. Mechanical
characteristics, in vitro degradation, and in vitro biocompatibility with murine pre-osteoblasts were also tested on the fabricated alloys. For in vivo examination of bone formation, osteointegration, and degradation rate,
the magnesium-based alloys were fabricated as small cylindrical pins
with a diameter of 2.7 mm and a height of 2 mm. The pins were implanted
in a critical-sized defect in a rat femur shaft (2.7 mm diameter and
2 mm depth) for 8 weeks and evaluated by micro-CT and histological
evaluation for bone growth and osteointegration. When compared to P-Mg
and P-MgHAP, micro-CT and histological analyses revealed that the
P-MgSrHAP group had the highest bone formation towards the periphery of
the implant and hence maximum osteointegration. When the removed pins
from the bone defect were analyzed using GIXRD, they displayed
hydroxyapatite peaks that were consistent with bio-integration. For
P-Mg, P-MgHAP, and P-MgSrHAP 8 weeks after implantation, in vivo degradation rates derived from micro-CT were around 0.6 mm/year,
0.5 mm/year, and 0.1 mm/year, respectively. Finally, P-MgSrHAP possesses
the requisite degradation rate as well as sufficient mechanical and
biological properties, indicating that it has the potential to be used
in the development/fabrication of biodegradable bioactive orthopaedic
implants.
Keywords